Rutishauser Lab
The Rutishauser Lab at UCSF is focused on understanding the mechanisms that promote the formation of CD8+ T cell immunity to viral pathogens in humans, and the impact of developmental stage on antiviral immunity.


We seek to:
- Understand the transcriptional and epigenetic regulation of HIV-specific CD8+ T cell exhaustion and the role of CD8+ T cells in establishing control of HIV in natural infection and after therapeutic intervention,
- Identify the molecular basis for - and clinical implications of - altered CD8+ T cell effector differentiation in early human development, and
- Characterize the broad immune responses elicited during acute infection and after vaccination that are associated with the development of protective antigen-specific immunity.
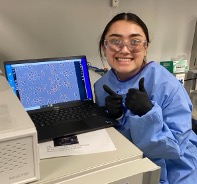
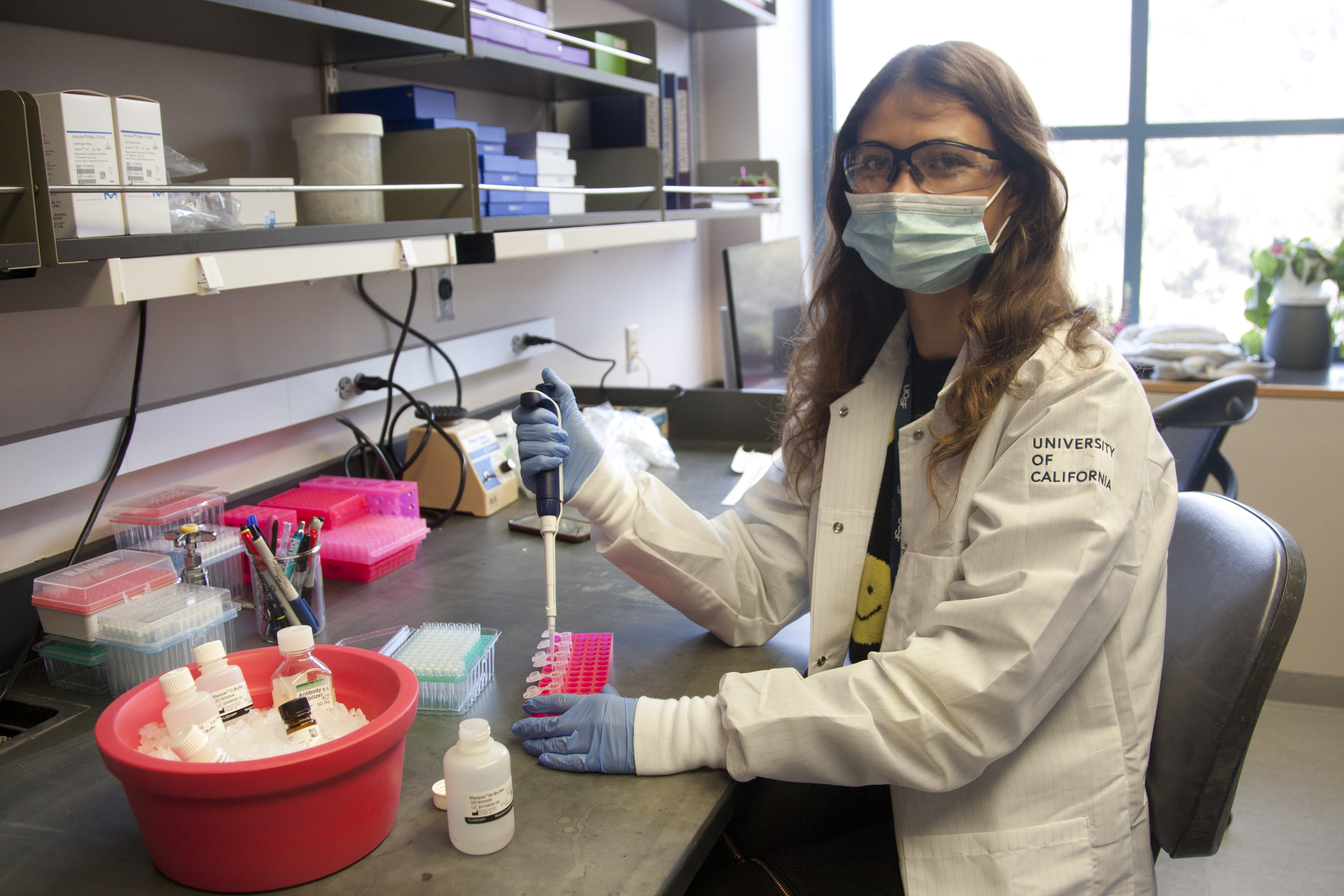
To do this, we apply high-dimensional single cell (flow and mass cytometry, single cell RNA/TCR sequencing) and genomics approaches (RNA-seq, ATAC-seq, WGBS, combined with genome editing of human primary T cells with CRISPR/Cas9).
The regulation of HIV-specific CD8+ T cell exhaustion. 37 million people world-wide are infected with HIV, a disease for which there is no cure. The majority of individuals infected with HIV have dysfunctional (exhausted) HIV-specific CD8+ T cells, a phenotype that is not reversed even after viral load suppression with antiretroviral therapy (ART). On the other hand, rare individuals who naturally control HIV infection to undetectable levels in the blood (elite controllers) have highly functional HIV-specific CD8+ T cells. Understanding how HIV-specific CD8+ T cell exhaustion and functional capacity are regulated is essential to inform the development of T cell-based therapies to control HIV, such as therapeutic vaccination and adoptive T cell therapies (e.g., CAR-T, TCR-T cells). Building on our close collaboration with the San Francisco-based SCOPE cohort, our lab studies:
- The transcriptional and epigenetic regulation of HIV-specific CD8+ T cell exhaustion: We have recently shown that the Wnt signaling transcription factor, TCF-1, which regulates stem cell-like transcriptional programs that counter antigen-specific CD8+ T cell exhaustion in mouse models of chronic infection and cancer, is expressed at high levels in functional HIV-specific CD8+ T cells in HIV elite controllers. Human primary T cells that we genetically engineered by CRISPR/Cas9 editing to express an HIV-specific T cell receptor (HIV TCR-T cells) and over-express TCF-1 demonstrate enhanced expansion capacity after in vitro peptide stimulation. However, this constitutive TCF-1 over expression also blocks cytotoxic effector differentiation. We are currently studying different approaches to targeting T cell stemness, or other pathways that regulate virus-specific CD8+ T cell differentiation, in order to enhance the ability of T cell-based therapeutic approaches to control HIV infection.
- The impact of therapeutic intervention on HIV-specific T cell differentiation state: Several T cell-based therapeutic approaches (e.g., therapeutic vaccines and adoptive T cell therapies) seek to promote HIV-specific T cell responses to overcome exhaustion and control the virus. However, the ability of these approaches to elicit and maintain functional T cell responses that can effectively target HIV remains unclear. We access highly unique samples from therapeutic vaccine and CAR-T cell clinical trials in people with HIV on ART (funded by the NIH, amfAR, and CIRM) to characterize the quality of the T cell responses elicited by these modalities, as well as the ability of these responses to control HIV after ART discontinuation.
Altered effector differentiation of naïve CD8+ T cells in early life. Infants have increased morbidity and mortality from infectious diseases compared to adults. We have found that, compared to their adult counterparts, early life human naïve CD8+ T cells have a profoundly altered transcriptional state, chromatin accessibility landscape, signaling response to T cell receptor stimulation, and effector differentiation compared to their adult counterparts. We are currently exploring how this altered differentiation potential impacts immunity to viral infection and vaccination early in development, including as part of a project to study CMV-specific CD8+ T cells in early human life with Dr. Maggie Feeney in our Division.
Systems immunology of acute viral infection and vaccination. Although Zika virus infection can lead to devastating morbidity to infants exposed in utero, infection in otherwise healthy adults is usually mild and is associated with the formation of a neutralizing antibody response. We analyzed longitudinal peripheral blood samples from Zika-infected adults by mass cytometry to explore how networked and coordinated immune responses during the acute phase of infection relate to the generation of durable neutralizing antibody responses (reported here). We are currently applying this systems immunology approach to characterize immunologic features associated with robust CD8+ T cell responses after therapeutic vaccination in HIV, and to characterize early life CD8+ T cell responses after immunologic perturbation.
A list of our publications in PubMed can be found here
Join us!

Are you interested in: T cell biology | human antiviral immunity | HIV cure research | early life immunity | single cell sequencing technologies | systems immunology | gene editing in T cells | strong mentorship | a fun and highly collaborative environment?
Click here to view active job postings in our lab and other labs in the UCSF Division of Experimental Medicine. We always welcome inquiries from interested postdoctoral fellow candidates and PhD students admitted to the UCSF BMS or UCB IDI programs.



